SIG Health Equity New Year news
Greetings and News

Hello again, from the WONCA Special Interest Group (SIG) on Health Equity. (
Photo: convenor, William Wong). The health equity group is still bustling with activity. As well as the enthusiastic discussions from our Health Equity Workshop at the WONCA Europe conference in Istanbul, we also encourage members to visit our newly affiliated journal:
International Journal for Equity in Health for up to date and exciting health equity research and news from around the world.
To start off, we will take a focus on Bangladesh, Uganda and Chinese Taipei in Global Focus (See: Global Focus below). As part of the affiliation, subscribed members are also entitled to a 20% discount on publications at the International Journal of Equity in Health.
As always we welcome contributions from any of our members. If you would like to subscribe to our mailing list, please direct your interest to:
[email protected]. Finally, we would like to wish everyone merry greetings for the upcoming holidays and celebrations for the New Year!
Reflection: WONCA Europe 2015: Health Equity Workshop, Istanbul
With 3,683 participants attending 289 oral presentations, 121 workshops, 30 symposia, and 1,403 poster displays; the WONCA Europe conference was surely a lively and bustling event. We on the special interest group (SIG) Health Equity team were delighted to be able to discuss with participants from many countries the importance of primary health care as a strategy to tackle health inequities in Europe. We would like to thank all those who took the time to attend our workshop as well as our SIG members who helped put this workshop together.
 Photo L to R: Dr W Halasa, Prof S Willems, Prof P O'Donnell, Dr U Chetty & Louisa Harding Edgar.
Photo L to R: Dr W Halasa, Prof S Willems, Prof P O'Donnell, Dr U Chetty & Louisa Harding Edgar.
Our workshop looked at different ways to improve equity in health with a focus on practice level strategies, and the training of health professionals. Through sharing of insights and experiences our enthusiastic participants suggested a diverse range of strategies at the consultation level. These included making use of trained interpreters to tackle language barriers with patients, and increasing consultation times. We also discussed the period of time spent in general practice training and how increasing contact with marginalized groups can promote empathy and awareness of the problems these patients face. Others suggested including health equity issues in the assessment of undergraduate students and GP trainees.
When we surveyed the workshop participants, we found that medical education was deemed to be the most important factor to reducing health inequity. This was a similar finding to the survey conducted at our previous workshop in 2014(1). In the coming year we hope to focus the work of the SIG on this very initiative and look forward to many interesting discussions on this topic of education.
Dr Patrick O’Donnell
Europe regional representative
A global focus on Health Equity
The first Global Focus will take a look at recent health equity related research from Uganda, Bangladesh and Chinese Taipei. Please feel free to visit our affiliated journal:
International Journal for Equity in Health for the full text.
Food for thought – income inequality and health
Income, as well as other measures of socioeconomic status has long been considered as a social determinant of health(5). Directly related to this is a study by Katz et al (2015) (6). They set out to assess the effectiveness of pay-for-performance schemes on childhood vaccination rates of families at different income levels. Interestingly, their control group (i.e. without pay-for-performance); found that the income-related inequities to vaccination rates increased over their study period. Essentially, the gap between the vaccination rates of the wealthy and the poor, although already existed at the start of the study period, worsened over time. Hence, the study shows how health interventions themselves can directly impact health outcomes as a result of income inequality. Aside from vaccinations, other health outcomes have also been assessed; such as mammograms and colorectal cancer screenings(7).
However the impact of income and socio-economic status on health been linked through many studies in differing socio-cultural contexts (8). A review by Picket & Wilkinson (2009) not only reveals this to be the case on a national level; but further this by demonstrating causally that the larger the income disparities within a country the more damaging the health and social consequences(9). This can be well demonstrated in Figure 1 (From Pickett & Wilkinson, 2015(10)). They explain that larger differences in income affects social distance (related to social hierarchy and difference in social status), and is likely to affect the health of its communities indirectly through the processes that manifest to generate social class across societies. Hence, that income inequality itself cannot be classed as a separate social determinant of health in its own right.
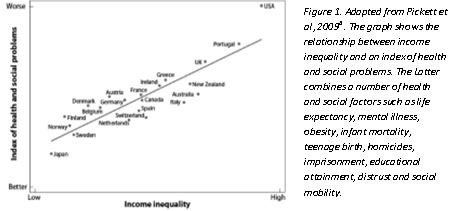
Figure 1. Adapted from Pickett et al, 2009(6) . The graph shows the relationship between income inequality and an index of health and social problems. The Latter combines a number of health and social factors such as life expectancy, mental illness, obesity, infant mortality, teenage birth, homicides, imprisonment, educational attainment, distrust and social mobility.
Publication of Interest
Contribution of Primary care to health: An individual level analysis from Tibet, China
Wang W., Shi L., Yin A., Mao Z., Maitland E., Nicholas S., Liu X.
Introduction: There have been significant improvements in health outcomes in Tibet, health disparities between Tibet and the rest of China has been greatly reduced. This paper tests whether there was a positive association between good primary care and better health outcomes in Tibet.
Methods: A validated Tibetan version of the Primary Care Assessment Tool (PCAT-T) was used to collect data on 1386 patients aged over 18 years old accessing primary care. Self-rated health (SRH) was employed to measure health outcomes. A multiple binary logistic regression model was used to explore the association between primary care quality and self-rated health status after controlling for socio-demographic and lifestyle variables.
Results: This study found that primary care quality had a significant positive association with self-rated health status. Among the nine domains of PCAT-T, family centeredness domain had the highest Odds Ratio (OR = 1.013) with SRH. Patients located in rural area, with higher education levels, without depression, and less frequent drinking were more likely to self-rate as “good health” compared with the reference group.
Conclusion: In Tibet, higher quality primary care was associated with better self-rated health status. Primary care should be much strengthened in future health system reform in Tibet.
References
1. Shadmi, E., Wong, W. C., Kinder, K., Heath, I., & Kidd, M. (2014). Primary care priorities in addressing health equity: summary of the WONCA 2013 health equity workshop. International journal for equity in health, 13(1), 104.
2. Hussain, S., Ruano, A. L., Rahman, A., Rashid, S. F., & Hill, P. S. (2015). From knowing our needs to enacting change: findings from community consultations with indigenous communities in Bangladesh. International journal for equity in health, 14(1), 1-9.
3. Wandera, S. O., Kwagala, B., & Ntozi, J. (2015). Determinants of access to healthcare by older persons in Uganda: a cross-sectional study. International journal for equity in health, 14(1), 26.
4. Chen, P. C., Tsai, C. Y., Woung, L. C., & Lee, Y. C. (2015). Socioeconomic disparities in preventable hospitalization among adults with diabetes in Taiwan: a multilevel modelling approach. International journal for equity in health, 14(1), 31.
5. 10 facts on health inequities and their causes. (2011, October 1). Retrieved December 8, 2015, from http://www.who.int/features/factfiles/health_inequities/en/
6. Katz, A., Enns, J. E., Chateau, D., Lix, L., Jutte, D., Edwards, J., … & Burland, E. (2015). Does a pay-for-performance program for primary care physicians alleviate health inequity in childhood vaccination rates?. International journal for equity in health, 14(1), 1-7.
7. Li, J., Hurley, J., DeCicca, P., & Buckley, G. (2014). Physician Response To Pay‐For‐Performance: Evidence From A Natural Experiment. Health economics, 23(8), 962-978.
8. Pickett, Kate E., Oliver W. James, and Richard G. Wilkinson. "Income inequality and the prevalence of mental illness: a preliminary international analysis." Journal of Epidemiology and Community Health 60.7 (2006): 646-647.
9. Pickett, K. E., & Wilkinson, R. G. (2015). Income inequality and health: a causal review. Social Science & Medicine, 128, 316-326.
10. Pickett, K. E., & Wilkinson, R. G. (2009). Greater equality and better health. Bmj, 339.
To remove your name from our mailing list, or if you have any questions or comments, please send e-mails to
[email protected].