A Nordic PhD: Clinical inertia or collective resistance?
General practitioners seem reluctant to follow guidelines for primary cardiovascular prevention.
A recently published PhD dissertation from Icelandic general practitioner Hálfdán Pétursson 1 may provide some answers to the long time conflict between general practitioners and cardiovascular specialists, on risk factor thresholds for primary cardiovascular prevention. Various studies have shown that general practitioners only follow the guidelines to a certain extent, and that recommended treatment goals are often not reached. Some authors have explained this in terms of physicians' inadequacy, whilst others have pointed out that at least part of the explanation is likely to lie in the nature of the guidelines 2.

Dr Hálfdán Pétursson
In one of the papers included in the thesis3 Pétursson and his collaborators have performed a modelling study demonstrating how adhering to the European guidelines from 20074 would translate in a practical sense to work load for general practitioners. They assumed that general practitioners were able to detect and respond appropriately to these guidelines, based on data from the Norwegian population based Nord-Trøndelag health survey (HUNT). This 1995-97 survey, comprised data on some 62,000 adults, which provides population data on blood pressure, cholesterol levels and a number of other potential relevant risk factor for cardiovascular disease. The authors summarise their findings on what work load this would imply for general practitioners in the county in a rather laconic way:
“Among individuals with blood pressure ≥120/80 mmHg, 93% (74% of the total adult population) would need regular clinical attention and/or drug treatment, based on their total CVD risk profile. This translates into 296,624 follow-up visits/100,000 adults/year. In the Norwegian healthcare environment, 99 general practitioner (GP) positions would be required in the study region for this task alone. The number of GPs currently serving the adult population in the study area is 87 per 100,000.”
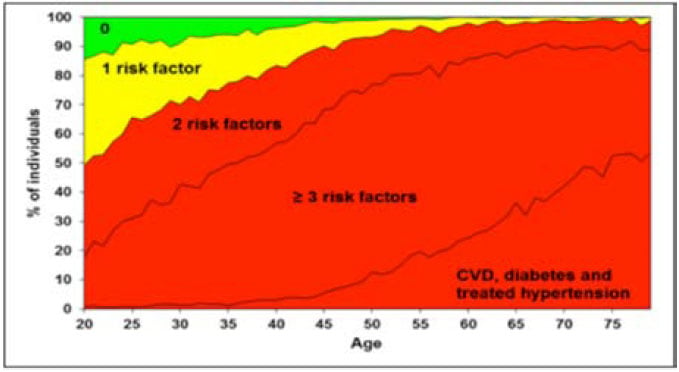
Can we as general practitioners accept these guidelines for CVD risk identification? A critical view at the 2007 European guidelines4, as applied to the Norwegian population in Nord-Trøndelag county, here showing point prevalence of individuals in each age group (20–79 years) who report established CVD disease or one or more of the risk factors studied (i.e. prehypertension or hypertension, high cholesterol, overweight or waist obesity, smoking, or close relatives with cardiovascular disease)5.
The study does not provide any information on what goes on in the heads of general practitioners, or to what extent they are aware of the massive discrepancies between guideline recommendations and their much Dr Hálfdán Pétursson lower intervention levels on cardiovascular risk factors. In some way (yet unknown), it seems like they translate these guidelines into something more “manageable”, since general practitioners obviously carry out a lot of medical work not related to cardiovascular prevention (as an understatement).
Most likely they manage their everyday clinical work by setting the risk thresholds for follow up or intervention on risk factors at a higher level than recommended by guidelines. At best, they will concentrate their work on the high risk segments, where the potential benefits of drug treatment are more indisputably documented. However, the low adherence rate to the guidelines may be interpreted as “clinical inertia”. Or – as some of us would say – silently demonstrating a collective resistance against guidelines unsuited for population based prevention 5. The authors summarize their views 3:
“The potential workload associated with implementing the 2007 European hypertension guidelines could destabilize the healthcare system in Norway, one of the world's most long- and healthy-living nations, by international comparison. Such a large-scale, preventive medical enterprise can hardly be regarded as scientifically sound and ethically justifiable, unless issues of practical feasibility and sustainability are considered in a transparent way.”
In his dissertation Pétursson also raises questions about prevention strategies, the balance between individual risk identification and interventions, and population based interventions (some echoes of the Geoffrey Rose classics6). But the main message from his analyses is that there is an urgent need for rethinking cardiovascular prevention in a broader public health perspective. The recently updated 2012 European guidelines for cardiovascular prevention7 make some minor modifications of their recommendations, but provide no better answer to this major question.
Prof Steinar Westin
General practitioner and professor of social medicine
Department of Public Health and General Practice
Norwegian University of Science and Technology
Trondheim, Norway
References:
- Pétursson H. The validity and relevance of international cardiovascular disease prevention guidelines for general practice. PhD dissertation. Trondheim: Department of Public Health and General Practice, Norwegian University of Science and Technology, 2012.
- Westin S, Heath I. Thresholds for normal blood pressure and serum cholesterol. BMJ 2005; 330: 1461-2 (editorial).
- Pétursson H, Getz L, Sigurdsson JA, Hetlevik I. Current European guidelines for management of arterial hypertension: Are they adequate for use in primary care? Modelling study based on the Norwegian HUNT 2 population. BMC Fam Pract 2009;10: 70.
- Mancia G, De Backer G, Dominiczak A, et al.: Guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007, 28 (12):1462-1536.
- Pétursson H, Getz L, Sigurdsson JA, Hetlevik I. Can individuals with a significant risk for cardiovascular disease be adequately identified by combination of several risk factors? Modelling study based on the Norwegian HUNT 2 population. J Eval Clin Pract 2009;15:103-9.
- Rose G. Sick individuals and sick populations. Int J Epidemiol 1985;14:32-8.
- European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). European Heart Journal doi:10.1093/eurheartj/ehs092.